Plantar Fasciitis in Runners: Symptoms, Causes, and Treatment

Running is more than just tying your shoelaces and heading out. It is a workout that engages a multitude of your lower body muscles that helps maintain your stride. A key focus area for runners is to increase their weekly mileage. However, to improve your aerobic fitness you need to go slow and gradually build up your strength and speed.
A sudden increase in physical activity can exert stress on your muscles, ligaments, and tendons, leading to inflammation and pain. Overuse injuries are common in runners across the spectrum and plantar fasciitis is one such condition. It is the most common cause of pain under the heel and accounts for 8% of running-related injuries. The silver lining is that it is manageable with early intervention.
What is plantar fascia and what is plantar fasciitis?
The plantar fascia is a fibrous band of tissue that runs from your heel to the toes. It supports the arch of the foot by acting as a tie-rod. It is an important component for weight-bearing and maintenance of gait while walking and running. Any inflammation in the plantar fascia is known as plantar fasciitis.
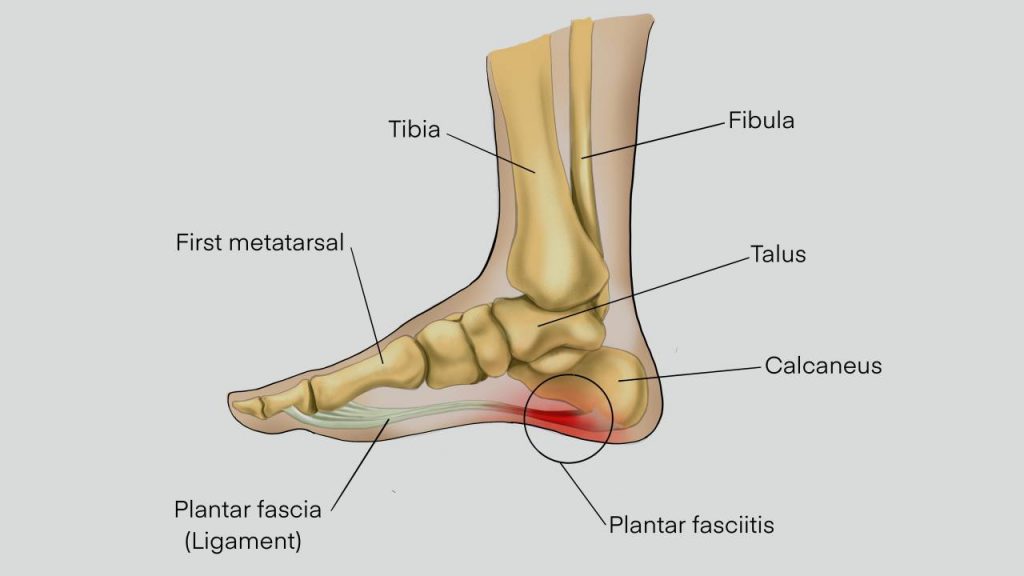
With plantar fasciitis, running becomes a challenge as repeated foot strikes can be painful and prevent normal healing. Repetitive stress can put excessive tension on the plantar fascia, and create microtears that eventually lead to inflammation. Degeneration of the tissue can happen over time.
What are the risk factors for plantar fasciitis?
1. Excessive load on the fascia in overweight and obese individuals can lead to failure of its weight-bearing mechanism, and cause tears and inflammation. It is reported that over 70% of individuals reporting plantar fasciitis tend to be overweight or obese.
2. Running on hard surfaces without proper footwear and adequate cushioning can cause the condition. Wearing improper shoes, ie, shoes that are uncomfortable and do not support your foot structure, can result in increased weight or pressure applied over different areas of the foot. Not wearing suitable and well-cushioned shoes, especially while running on hard surfaces, may result in reduced shock absorption, which will increase the impact of forces from the hard surfaces to your feet.
3. Prolonged periods of standing.
4. Excessive running without proper conditioning and graded increase in training.
Tight calves and Achilles tendon (the tendon connecting the calf muscle to the heel), flat foot and high arched foot are other risk factors for the development of plantar fasciitis.
Also read: Running Surfaces: Where Should You Run?
Symptoms of plantar fasciitis
1. Plantar fasciitis typically appears during exercise or a day after a stressful activity
2. Sharp, stabbing pain, on the inside bottom of the heel
3. The pain is severe in the morning and typically makes the athlete squirm while placing the first foot on the ground after getting up from bed
4. The pain gradually reduces over the next few minutes to hours due to “thawing” of the foot
5. The pain may increase towards the end of the day due to prolonged stress on the feet
Treatment
One of the primary things to do in plantar fasciitis is to reduce stress on the area. However, the pain and discomfort can limit your activities. If you have plantar fasciitis, you can try the following:
1. RICE: Rest, Ice, Compression, and Elevation
- If you experience heel pain while running, it is best to stop.
- Rest your feet, ice the heel for 10 mins, 2-3 times a day, elevate the foot, and gently massage the area.
- If the pain persists, consult a physiotherapist as aggravated cases of plantar fasciitis can take time to heal and cause intense pain.
- Avoiding standing, walking, and running for prolonged periods.
2. Shoe modification
- Some individuals may find their symptoms getting better with a change of shoes. Opt for shoes that fit you well. Avoid ill-fitting shoes, especially ones that are too small/ tight as it can exacerbate the pain.
- Shoes with thicker and cushioned midsoles and motion control shoes for individuals with flat feet can help in reducing foot pain associated with standing or walking for long periods.
- Avoid wearing worn-out shoes as they tend to lose their shock-absorption property over time.
- Mechanical corrections like arch taping, over-the-counter arch supports, and custom orthotics can be used to provide better foot support and reduce stress. Softer heel inserts or supportive shoes allow more movement with less irritation.
3. Exercise
- After the initial period of rest, it is recommended to gradually start stretching the foot and Achilles tendon to help prevent tightness.
- Stretching and strengthening exercises for the foot can help in reducing plantar fasciitis. Some of the helpful exercises include:
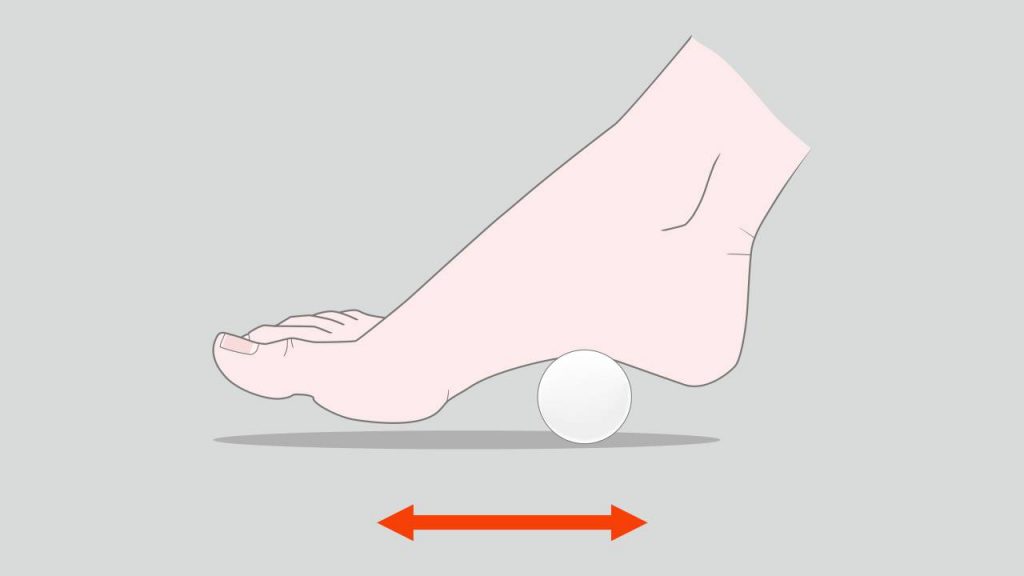
Ball rolling
In a seated position, roll a ball, eg, a tennis ball with the arch of your affected foot. Once you are comfortable doing this, try doing the same exercise while standing.
Toe stretch
As you sit, extend the affected leg and pull your big toe towards the ankle and away from the floor. Hold the stretch for 15-30 seconds and repeat 2-4 times.

Calf stretch
Stand facing a wall, place your hands on the wall, keep the affected leg a step behind the other leg. The heel of the back should touch the floor as you bend the front knee to feel a stretch on the back leg. Hold the pose for 15-30 seconds and repeat 2-4 times.

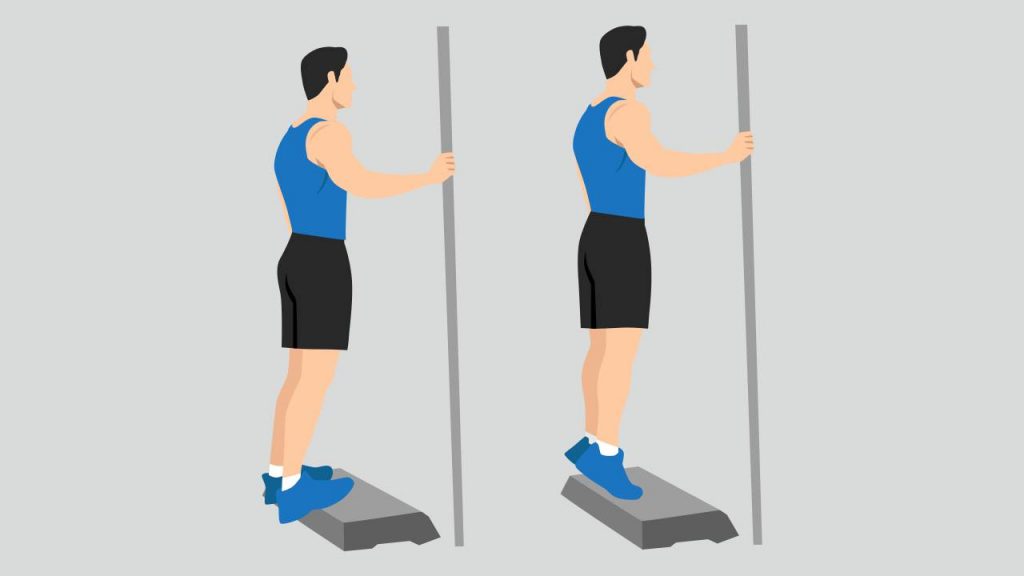
Calf stretch
Stand on a step and as you relax your calf muscles, slowly lower your heels below the edge of the step. Hold the stretch for 15-30 seconds and then slowly tighten the calf muscle as you get your heel back up. This can be repeated 2-4 times.
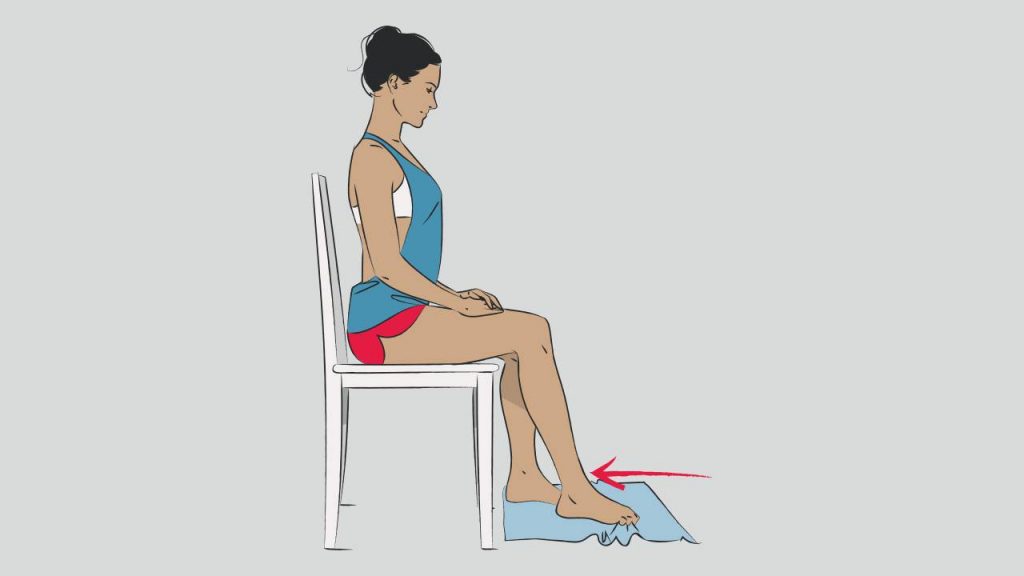
Towel curl
Keep a towel on the floor in front of you when you are in seated position. Place the affected foot on the towel and use your toes to scrunch the towel towards you and then push the towel away from you using your toes.
4. Medication
- Painkillers that can be taken orally may help in some cases. However, any medications should be taken after consulting a physician.
- In severe cases, doctors may recommend injection of local steroids.
What can you do to prevent it?
1. Avoid a sudden increase in your mileage or speed. An overuse injury is a primary cause for most running-related injuries and especially plantar fasciitis. A graded increase in training is the best way to avoid sports-related injuries including plantar fasciitis.
2. Runners, especially those who run regularly on hard surfaces, should wear well-cushioned shoes with arch support that can help better tackle all that pounding on concrete roads than shoes with hard soles and little arch.
3. Old footwear is a recipe for foot problems as the shoe loses its support. Be sure to change your footwear every 500-800km, earlier if you are heavier.
4. Building up foot strength supports the arch, and flexible calves and Achilles disperse force and take pressure off the plantar fascia.
5. Performing a good warm-up before and stretching after workouts may help in the flexibility of plantar fascia and reduce the chances of injury.
6. Maintaining a healthy body weight means less impact and stress on the foot.
To prevent plantar fasciitis, runners should wear appropriate running shoes, follow graded training modules, and maintain healthy body weight. In case the problem persists despite taking adequate precautions, seek the advice of a physiotherapist or a physician.
References
1. Menon N, Jain J. Plantar fasciitis: A review. Indian J Pain 2018; 32: 24.
2. League Alan. Current Concepts Review: Plantar Fasciitis. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society 2008; 29: 358-66.
3. Rosenbaum AJ, DiPreta JA, Misener D. Plantar heel pain. The Medical Clinics of North America 2014; 98: 339–52.
4. Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician 2011; 84: 676-82.
5. Cutts S, Obi N, Pasapula C, et al. Plantar fasciitis. Ann R Coll Surg Engl 2012; 94: 539-42.
6. Trojian T, Tucker AK. Plantar Fasciitis. Am Fam Physician 2019; 99: 744-50.
7. Plantar Fasciitis: Exercises to Relieve Pain. Michigan Medicine, University of Michigan. https://www.uofmhealth.org/health-library/tr5853 (accessed Apr 15, 2021).